Benefits of
Joining DPSC
No hassle claims submission – DPSC is the payor for all claims for DPSC plan members. Claims come directly to DPSC via EDI or Paper.
Get paid quickly: As the payer for all claims, DPSC pays all clean claims between 15 to 30 days from receipt. DPSC offers EFT payments or paper checks.
We do the leg work: We will assist with credentialing documents submission and keep you posted along the way. Once credentialed DPSC will ensure you are listed as an In-Network provider on the Health Plan provider search site.
Excellent Customer Service: We pride ourselves on building strong relationships with our network providers. You will always speak to a live person when you call DPSC for assistance.
No network or unexpected fees: DPSC needs your practice participation to service health plan members, so our partnership is completely free.
Access to exclusive membership: Unless you are a DPSC In Network provider, you will not be able to provide services or be reimbursed for DPSC plan membership. Our Health Plan partners contract only with DPSC to provide services to specific membership plans.
I have been working with DPSC since 1994. They are committed to our success as a company as if it were their own. Todd and his team go over and above day in and day out. And the fact you can speak with a person is priceless! Thank you, DPSC for making my job easier! It is always a pleasure to deal with you and your staff!
Health Plan Contracts
and Members

Aetna Medicare HMO/DNSP

Florida Healthcare Plans

Aetna Better Health

Humana HMO
Claims Submission
Made Easy
DPSC is the payor for all claims for services rendered to DPSC plan membership. As a DPSC Network Provider, you will enjoy our hassle-free claims submission and reimbursement process. DPSC offers EDI and Paper transactions and allows providers to be paid via EFT or paper checks. We do our best to make it easy!
Have a claims question? DPSC prides ourselves on Customer Service and building relationships with the Providers we work with. You’ll always speak with a live person when calling in with questions and our claims team responds quickly to email inquiries. We know your time is valuable. And you won’t have to wait months to be reimbursed for your services. DPSC’s reimbursement turnaround time is less than 30 days for clean claims submitted to us.
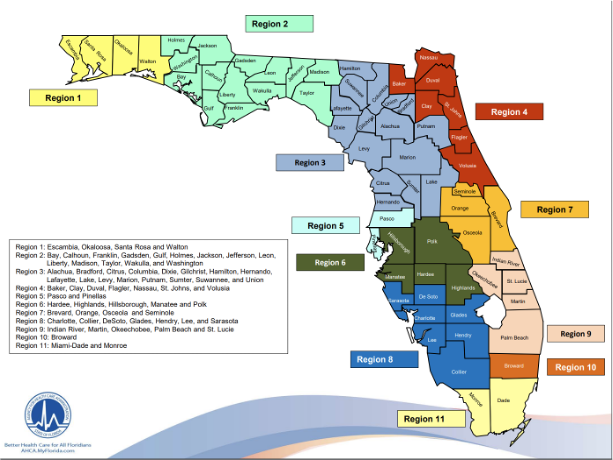
Florida Regions Where
Health Plans are Located
Aetna Medicare HMO Plans
Statewide/All Regions in Florida
Aetna Better Health Medicaid and Healthy Kids Medicaid Plans
Statewide/All Regions in Florida
Humana Medicare Gold Plus and Honor HMO plans
Region 1, Region 3, Region 4, Region 7, Region 8
Florida Health Care Plans
Select counties in Region 4 and Region 7<
Aetna POS, Commercial and Individual and Family Plans
Statewide